Media
Contact
Communications Specialist
Faculty of Engineering
Spencer Engineering Building
Room 2072
Western University
Tel: 519-661-2111 ext. 87015
Email: engineeringcomms@uwo.ca
New research helps ‘customize’ cochlear implants to the individual
Individuals who suffer from profound hearing loss depend on cochlear implants to aid in having conversational speech or listening to music, and when it comes to the use of cochlear implants, there is no “one-size-fits-all” method.
This is why, last year, Hanif Ladak, Professor, Department of Electrical and Computer Engineering (jointly appointed with the Department of Medical Biophysics), his surgical collaborator Dr. Sumit Agrawal (Otolaryngology – Head & Neck Surgery), and their team, including collaborators from the Uppsala University Hospital in Sweden, created a tool that would “ fine tune ” cochlear implants to ensure that unique anatomy was less of an obstacle for patient hearing.
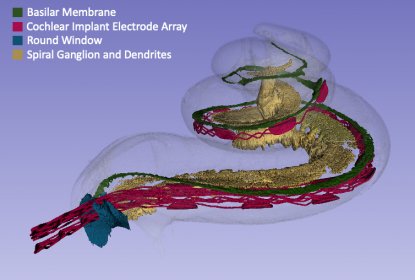
Rendering of a 3D synchrotron-based image of an implanted cochlea
Cochlear implants work by implanting an electrode along the length of the cochlea, the part of the inner ear responsible for converting sound to neural signals. The electrode can stimulate the sensory cells.
Prior to last year’s mapping tool, understanding what cells to stimulate was far more challenging.
“The sensory cells inside the cochlea are spatially distributed according to frequency, and this spatial distribution depends on the overall anatomy of each patient. To improve pitch perception, the electrode should be programmed after surgery to stimulate cells that best match the frequency content of the sound signal,” said Ladak. “Currently, programming is done blindly since the spatial relationship between the electrode and particular cells is not known given that post-surgical imaging is not the standard of care and because of the low resolution and contrast of clinical images.”
“Because of these limitations, the implant was often programmed using a ‘one-size-fits-all’ approach towards an average anatomy with the outcome that speech and music did not sound natural to some patients and hampered speech communication and music enjoyment. By introducing imaging and using machine learning to estimate cell distribution, we are now able to tune an implant to each patient’s specific anatomy to achieve high-quality sound rendering,” he added.
Using imaging data gathered with a tool they pioneered last year, Ladak and his team are now taking the research one step further. In addition to tuning the implant to each patient’s anatomy, they will optimize the physical design of the implant’s electrode to best utilize their discoveries about cochlear micro-anatomy.
“By using our unique database of images, we’ll be able to design highly detailed computer models and once they are validated, they can be used to optimize the shape and sizing of the electrodes on an individual basis,” shared Ladak.
This new development means cells are better targeted for stimulation and this will result in improved tuning of the electrode to the patient's specific micro-anatomy allowing for improved hearing.
The World Health Organization estimates that by 2050, over 700 million people – or one in every ten people – will have disabling hearing loss.
As the criteria expand for individuals who can receive a cochlear implant, Ladak’s work becomes more crucial. “I'm hoping that some of the technology that we've developed just over the last five years will be translated to practice within the next three or four years.”
“Individuals who have a profound loss of hearing and for whom hearing aids and other technologies don't work will be positively impacted by our research in terms of access to education, future employment, and social activities,” he added.

