Research
Musculoskeletal Imaging
Project: 3DUS to Monitor Synovitis in Patients with CMC OA
Graduate Student: Carla Du Toit
The 1st carpometacarpal (CMC) joint of the thumb is a very common site for osteoarthritis, affecting approximately 11% and 30% of middle aged (50-60 years old) men and women world-wide. 1st CMC osteoarthritis (CMC OA) can lead to weakness, laxity of the joint, pain, disability and ultimately loss of quality of life. The current practice for diagnosing 1st CMC OA is plain x-ray radiographs and a clinical examination, which includes patient history, examination of patient symptoms and stress tests such as the grind and distraction tests. For these tests, a positive result is an indicator for the presence of synovitis (swelling) in the joint.
CMC OA is traditionally imaged using radiographs, which present several limitations when examining joint structures. The most relevant limitation for CMC OA is the inability to discriminate between soft tissue pathologies (abnormal changes) which can contribute to symptoms experienced by patients such as pain.
3-dimensional ultrasound (3-D US) is a medical imaging modality that utilizes high frequency sound waves to capture real-time images of internal anatomical structures. 3-D US may provide a fast and efficient method from overcoming the limitations presented by current diagnostic practices and play a role detecting sources of pain and disability in CMC OA patients. The purpose of this study is to develop and validate a 3-D US device for CMC OA patients, which can accurately and precisely measure synovial tissue volume to monitor synovitis (swelling) of the CMC joint.
Patients who are currently being treated at the Roth McFarlane| Hand and Upper Limb Centre for 1st CMC pain will be recruited for this study. The participants will undergo bilateral imaging of their hand and wrist using 2-D US, 3-D US and some patients will be chosen for magnetic resonance imaging. Patients will also be asked to complete an AUSCAN questionnaire, a visual analogue scale questionnaire and a series of pinch grip tests to determine patient perceived pain and disability.
Project: 4DCT to examine scapholunate ligament injuries
Graduate Student: Sydney Robinson
Traumatic injury of the scapholunate ligament can lead to long-term pathologies, such as scapholunate advanced collapse (SLAC), which is a form of degenerative arthritis. Symptoms of SLAC include pain and abnormalities of bone movement, without external markers. Four-dimensional computed tomography (4DCT) is able to capture the abnormal bony movements that are otherwise missed with current imaging procedures. Current diagnostic tools are limited to radiographs, the shift test [2], and the Terry Thomas sign [3]. Four-dimensional computed tomography (4DCT) can be used to accurately diagnose SLAC by illuminating features in bone movements during functional tasks. Early and accurate detection is the key to proper treatment and preventing further joint degeneration. The purpose of this study is to develop a wrist positioning device for scapholunate injury, which can apply functional loads and simulate activities of daily living (ADL), and to use 4DCT to determine how scapholunate instability leads to progressive joint degeneration.
A series of participants (n=30, male: 15) who are currently being seen at the Roth McFarlane | Hand and Upper Limb Centre for wrist pain associated with potential scapholunate instability and a cohort of healthy participants (n=30, male: 15) will be recruited. The participants will undergo unilateral imaging of the wrist using a 4DCT scanner while performing various ADLs (i.e. push-up, dart throwers motion, etc.). Using dynamic CT scanning, it is possible to render 3D videos of the carpal bones continuously and to examine subtle changes in contact mechanics and kinematics that are present due to the potential scapholunate instability. Early diagnosis of scapholunate injuries can prevent the onset of osteoarthritis (OA) by providing physicians with the opportunity for early detection and intervention. Novel information on scaphoid movement can assist: in designing and developing wrist arthroplasty tools and procedures; surgeons in positioning the carpal bones when performing partial wrist fusions; in developing better techniques for scapholunate ligament repair and reconstruction [5]
Project: Dynamic 4DCT to examine the effects of mal-united distal radius fractures on carpal contact mechanics
Graduate student: Puneet Kaur Ranota
Distal radius fractures (DRF) are common orthopedic injuries and one of the major complications following a DRF is malunion. Planar x-rays are used by researchers and doctors to evaluate wrist joints, but they are not always precise and limited to two dimensions. Three-dimensional (3D) computed tomography (CT) can be used to look at the wrist joints in three dimensions, but it is limited to static frames. Four-dimensional computed tomography (4DCT) allows for dynamic assessment of the joint mechanics. This novel imaging technique provides a movie of bones in the wrist. The purpose of this investigation is to examine the way wrist bones are moving and contacting following a DRF and the possibility of abnormal wear and tear over time. These findings will allow us to better understand the relationship between joint alignment following a wrist fracture and the associated long-term clinical outcomes. Additionally, these findings will benefit society by developing tools to predict the risk of developing arthritis and it will help doctors determine when surgery post fracture is necessary to prevent the arthritis of the hand and wrist, pain and disability.
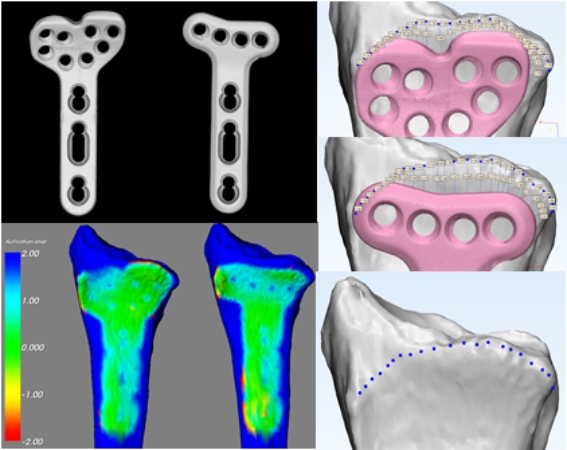
Patients who have suffered from a DRF who were treated at the Roth | McFarlane Hand & Upper Limb Centre were identified and contacted. The inclusion criteria included unilateral wrist fracture and the exclusion criteria included plate, and pins (metal). Using the 4DCT scanner, wrists of participants were scanned in 2 static positions (pronation and supination) and 3 kinematic motions (full pronation to full supination, full wrist flexion to full extension, and radial deviation to ulnar deviation). Three-dimensional reconstructions of the wrist bones were created using a threshold-based semiautomatic segmentation. A previously developed inter-bone distance algorithm was used to measure relative 3D joint space reduction over time in the joints. Repeated measures ANOVA will be conducted to identify significant differences.
Project: Sex-linked Differences in Distal Radius Morphology: Implications of Volar-locking Plate Design
Graduate Student: Madeline Perrin
Distal radius fractures are one of the most commonly occurring fractures in the human
This project focuses on determining if
Project: 3D Ultrasound to Investigate Effusion Synovitis in the Hand and Wrist
Graduate Student: Carla Du Toit
The 1 st carpometacarpal (CMC) joint of the thumb is a very common site for osteoarthritis, affecting approximately 11% and 30% of middle aged (50-60 years old) men and women world-wide. 1 st CMC osteoarthritis (CMC OA) can lead to weakness, laxity of the joint, pain, disability and ultimately loss of quality of life. The current practice for diagnosing 1 st CMC OA is plain x-ray radiographs and a clinical examination, which includes patient history, examination of patient symptoms and stress tests such as the grind and distraction tests. For these tests, a positive result is an indicator for the presence of synovitis (swelling) in the joint.
CMC OA is traditionally imaged using radiographs, which present several limitations when examining joint structures. The most relevant limitation for CMC OA is the inability to discriminate between soft tissue pathologies (abnormal changes) which can contribute to symptoms experienced by patients such as pain.
3-dimensional ultrasound (3-D US) is a medical imaging modality that utilizes high frequency sound waves to capture real-time images of internal anatomical structures. 3-D US may provide a fast and efficient method from overcoming the limitations presented by current diagnostic practices and play a role detecting sources of pain and disability in CMC OA patients. The purpose of this study is to develop and validate a 3-D US device for CMC OA patients, which can accurately and precisely measure synovial tissue volume to monitor synovitis (swelling) of the
CMC joint.
Patients who are currently being treated at the Roth McFarlane| Hand and Upper Limb Centre for 1 st CMC pain will be recruited for this study. The participants will undergo bilateral imaging of their hand and wrist using 2-D US, 3-D US and some patients will be chosen for magnetic resonance imaging. Patients will also be asked to complete an AUSCAN questionnaire, a visual analogue scale questionnaire and a series of pinch grip tests to determine patient perceived pain and disability.
Project: Radiocarpal vs Midcarpal Joint Contribution to the Flexion/Extension Motion of the Wrist with Identification of Healthy Center of Rotation
Graduate Student: Elizabeth Norman
The wrist is a very complex joint with multiple articulations, muscles, tendons, and ligaments present that afford the wrist with its wide range of motion. Due to its complex nature wrist injuries are common and these injuries may result in impaired overall function of the joint. To treat these injuries an accurate biomechanical model is needed to target treatment strategies and obtain a thorough understanding of the healthy wrist motion. Kinematics can be used to characterize healthy wrist motion such as joint contribution and center of rotation (COR); these attributes are essential for proper identification of healthy wrist motion.
Ten healthy participants have been recruited to the Roth McFarlane | Hand and Upper Limb Centre where their wrists were scanned with the use of a four-dimensional computed tomography scanner (4DCT). This scanner allows us to capture three dimensional images over a period of time and thus the participants completed two ‘passes’ of motion from extreme extension to extreme flexion and the reverse in 8 second intervals. These scans gave us the ability to analyze the contribution of each joint throughout the motion with the use of instantaneous helical axes. In addition, the COR was also determined for all participants and with a 95% confidence interval a healthy range for COR was determined. This study has very important applications for basic biomechanics and will lead to better treatments as it describes the wrist in its native state.
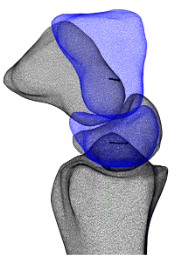
Project: Longitudinal Effects of Scapholunate Instability on Two Image-Based Biomarkers and Chronic Pain: Utility of Quantitative CT
Graduate Student: Lauren Straatman
Scapholunate injuries (SL) are the most common type of ligamentous wrist injury that commonly leads to instability, pain and functional disability, having a serious impact on patients quality of life. The population most commonly impacted by SL injuries is a young (approximately 40 years of age), male population with a history of working in manual labour. If an SL injury is left untreated, the resultant consequence is a form of secondary OA known as Scapholunate Advanced Collapse (SLAC). Scapholunate advanced collapse is responsible for degenerative changes to the articular cartilage that commonly leads to increased wear between the bones. These changes are often associated with lasting pain and disability, and considering the prevalence in a young, working population, may lead to decades of impairment. The stages of SLAC are well-defined, transitioning from stage 1 (the most mild stage of SLAC), to stage 3 (the most severe stage, encompassing the whole radiocarpal articulation). Treatment options vary according to the stage of SLAC, however there is no cure for SLAC and the most common end-stage treatment involves salvage procedures, such as carpal fusion.
Current literature has focused on joint mal-tracking as the underlying mechanism leading to post-traumatic OA. However, other studies have demonstrated that some malalignment within the joint is tolerated, without arthritic progression. Specifically, malalignment should be considered a gradient risk of poor outcomes rather than an all-or-none phenomenon. Anatomically, cartilage is avascular and aneural, meaning that there are no blood vessels or nerves that supply the articular cartilage structure. This leads us to a very important question – if the articular cartilage is avascular and aneural in nature, why does increased wear on the cartilage cause some people to experince chronic pain and typical arthritic patterns following wrist trauma, while other people do not?
Current research on the knee is pointing towards a depth-specific imaging technique using quantitative computed tomography (QCT). QCT has been used to analyze depth-specific volumetric bone mineral density (vBMD) as it relates to depth from the subchondral surface. These depth-specific imaging techniques have the potential to make distinctions between subchondral bone layers, which researchers are turning to as potential contributors to the pain experience in myriad MSK injuries due to the vascularity of the subchondral bone. Although this phenomenon has not yet been studied as extensively in the wrist, we believe depth-specific changes in the subchondral bone will help explain underlying biological mechanisms of post-traumatic OA and pain following SL injuries.
The purpose of our work is to prospectively and retrospectively analyze quantitative changes in subchondral vBMD following unilateral SL injuries, and the relationship between altered joint contact and subchondral bone. Sixty participants will be recruited for our study; n = 30 with a current, unilateral SL injury (prospective cohort) and n = 30 with a previous SL injury (retrospective cohort; 5+ years post injury), through the Hand and Upper Limb Center (HULC) at St. Joseph’s Hospital. All participants will undergo static CT scans accompanied by a calibration phantom used to estimate relative vBMD, and kinematic four-dimensional CT scans while performing a range of motion, to estimate joint contact. Participants will also undergo a battery of self-reported pain questionnaires in an attempt to capture the patients pain experience.
Locomotion and Human Movement
Project: Evaluating the Hand Forces of Golfers with and without Hand Arthritis
Graduate Student: Sara Holland
With diagnosed arthritis affecting 1 in 5 adults in Canada along with an increasingly aging population, playing sports such as golf becomes difficult. The grip of a golf club is the only contact point between the player and the club, making the player’s gripping force and the golf grip itself an important elements of the game. However, the golf grip is the most overlooked piece of equipment in a player’s bag. Comprehensive examinations have not been done on current golf grips and a small amount of arthritis golf grips have recently been marketed but are not based on empirical measurements or been properly tested to determine their effectiveness at reducing joint pain in a players hands. Therefore, the purpose of this study is to systematically analyze the hand forces produced from various golf grips at the hand-grip interface in individuals with and without hand arthritis.
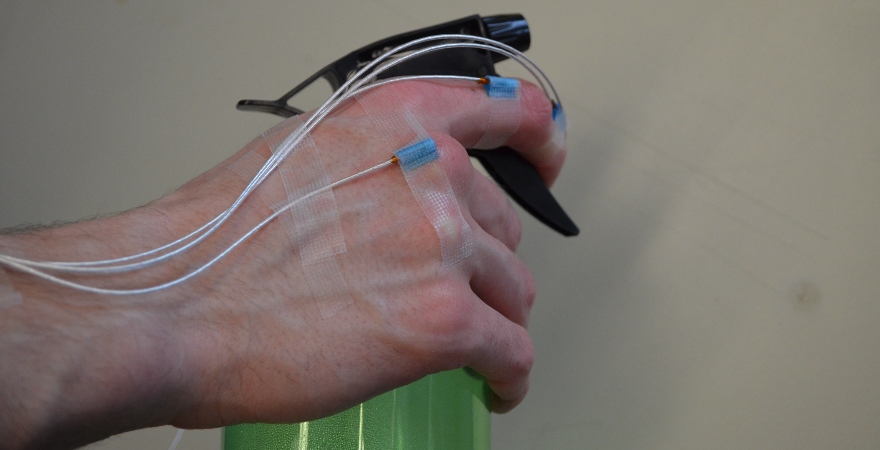
The new wearable sensor technology system designed by Pressure Profile Systems

Project: Comparison of Surface Mounted and Bone Mounted Electromagnetic Tracking Methods
Graduate Student: Ahmed Tanashi
Hand osteoarthritis is a common type of arthritis that causes pain, stiffness, and swelling of the hand and fingers. This contributes to difficulties in performing daily tasks such as opening doors or dressing oneself. The kinematics of the finger
The 3D Guidance trakSTAR electromagnetic tracking system is being used with the model 180 sensors, made by Ascension Technology Corporation, to evaluate finger kinematics during the study. An in vitro study is being conducted to directly compare skin mounted to bone mounted
Injury and Rehabilitation
Project: Evaluation of Hand Forces during Activities of Daily Living
Graduate Student: Michael L. Riddle
Hand-Osteoarthritis affects over 20% of the adult population in Canada. The significant consequences of osteoarthritis include reduced hand function and pain in the hands. Current clinical guidelines prescribe joint protection programs (JPP), which are self-management strategies to help patients with arthritis reduce pain and preserve joint function. However, current JPP
To achieve these objectives, finger forces are measured using wearable finger force sensors developed by Pressure Profile Systems, called Finger Tactile Pressure Sensors (FingerTPS). These two research objectives will be achieved over the course of two studies. For the first, both healthy participants and participants with hand arthritis are being recruited to perform 17 activities of daily living while wearing these sensors. Comparisons in the range of applied forces between healthy participants and those with arthritis can then be made to determine if there is a significant difference. For the second study, participants with arthritis are being recruited to perform the same 17 activities, both with and without the use of JPP to determine the effectiveness of JPP