For Patients
3D Ultrasound to Investigate Effusion Synovitis in the Hand and Wrist
3D Ultrasound to Investigate Effusion Synovitis in the Hand and Wrist
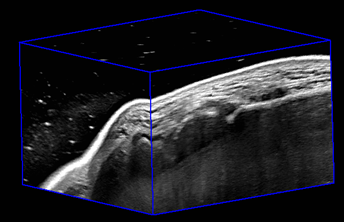
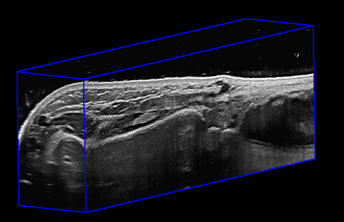
We wanted to develop and validate a new 3-dimensional ultrasound machine to see if it would be able to measure the amount of swelling (synovitis) seen in the joints located at the base of the thumb (called the 1st carpometacarpal joint) and in the wrist (radiocarpal joint) in patients who are experiencing pain.
|
1st CMC |
Radiocarpal Joint |
What is the problem?
Hand osteoarthritis (HOA) is a progressive joint disease that causes degradation of the soft found between the bones of the joint and is the cause of considerable pain and disability for many individuals, leading to inability to perform activities of daily living. Studies of elderly populations have estimated that the prevalence of hand OA ranges from 44% to as high as 92% in certain populations. The radiocarpal joint of the wrist and base of the thumb (1st CMC) are very common sites for arthritis in the hands. Thumb arthritis specifically affects approximately 11% to 33% of middle-aged men and women, respectively. Current methods of diagnosis include a clinical examination and plain x-ray radiographs, which are unable to detect subtle changes in soft tissue structures that might be the cause of pain and disability in patients. The biggest problem faced with radiographs is that the amount of structural damage seen on the films does not always correlate with the intensity of patient symptoms. 2-dimensional ultrasound (2-D US) has been used in clinics to monitor swelling and joint health and is readily available and inexpensive. The problem with 2-D US is that it uses 2-D images of structures that are actually 3-dimensional, and the quality of these images are highly dependent on the skill of the person operating the machine. However, 3-dimensional (3-D) ultrasound is an imaging method that overcomes the limitations of 2-D US and radiography by providing 3-D images of soft tissue structures and enabling clinicians to quantitatively characterize and monitor changes in disease progression. The purpose of this study is to examine the use of 3-D US to measure the volume of swelling observed in the 1st CMC and radiocarpal joints of patients who present with pain in that location.
How will the team study the problem?
Ten 1st CMC and ten wrist arthritis patients receiving treatment for pain from the Roth McFarlane| Hand and Upper Limb Centre will be recruited as well as five healthy volunteers. These participants will have images taken of their both CMC or wrist joints using 2-D US, 3-D US and some participants will be randomly chosen to have magnetic resonance images acquired. Participants will also be asked to fill out two surveys related to perceived pain and will be asked to perform pinch grip test to assess functional outcomes related to the thumb. The images will be used to find the volume of the synovial tissue swelling using software developed in Dr. Aaron Fenster’s lab. The synovial tissue volumes acquired will be compared to the results of the questionnaires, functional tests and previously acquired radiographic findings to determine if there is a relationship between synovial tissue volume and the intensity of pain experienced by patients.
Cited Sources:
Public Health Agency of Canada (PHAC). Life with arthritis in Canada: a personal and public health challenge. Ottawa (ON): PHAC; 2010 [cited 2019 Mar 20]. Available from: https://www.canada.ca/en/public-health/services/chronic-diseases/arthritis/life-arthritis-canada-a-personal-public-health-challenge.html
Dias, R., Chandrasenan, J., Rajaratnam, V., & Burke, F. D. (2007). Basal thumb arthritis. Postgraduate medical journal, 83(975), 40–43. https://doi.org/10.1136/pgmj.2006.046300
Klippel JH, Weijand CM, Wortmann RLHochberg MC. Osteoarthritis – clinical features and treatment. In: Klippel JH, Weijand CM, Wortmann RL, eds. Primer on the rheumatic diseases. 11th edn. Atlanta: Arthritis Foundation, 1997:218–21
Li, W. (2013). Carpometacarpal osteoarthritis of the thumb. Canadian Medical Association Journal (CMAJ), 185(2), 149–149. https://doi.org/10.1503/cmaj.111444
Maheu E, Altman RD, Bloch DA, Doherty M, Hochberg M, Mannoni A, Punzi L, Spector T, Verbruggen G, Carr A, Cicuttini F, Dreiser RL, Haraoui BP, Hart D, Pelletier J-P, Ramonda R, Rovati L. Design and conduct of clinical trials in patients with osteoarthritis of the hand: recommendations from a task force of the Osteoarthritis Research Society International. Osteoarthritis Cartilage. 2006;14:303–322. doi: 10.1016/j.joca.2006.02.010
Dahaghin S,Bierma-Zeinstra SM, Hazes JM, et al. Clinical burden of radiographic hand osteoarthritis: a systematic appraisal. Arthritis Rheum 2006;55:636–47
Longitudinal Effects of Scapholunate Instability on Two Image-Based Biomarkers and Chronic Pain: Utility of Quantitative CTRadial Deviation Imaging
Longitudinal Effects of Scapholunate Instability on Two Image-Based Biomarkers and Chronic Pain: Utility of Quantitative CT
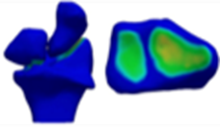
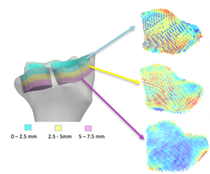
We sought out to understand the mechanisms underlying pain and disability following a common injury in the hand: scapholunate injuries. This type of injury is responsible for pain and disability for up to years and may also lead to a secondary form of osteoarthritis. Using a novel imaging technique (quantitative CT), we will be studying the amount of contact between the carpal bones and the underlying subchondral bone density, as potential biomarkers for pain and disability.
|
CT Scan |
Joint Contact Area |
Subchondral Bone Density |
What is the problem?
Scapholunate injuries (SL) are the most common type of ligamentous wrist injury that commonly leads to instability, pain and functional disability, having a serious impact on patients quality of life. The population most commonly impacted by SL injuries is a young (approximately 40 years of age), male population with a history of working in manual labour. If an SL injury is left untreated, the resultant consequence is a form of secondary OA known as Scapholunate Advanced Collapse (SLAC). Scapholunate advanced collapse is responsible for degenerative changes to the articular cartilage that commonly leads to increased wear between the bones. These changes are often associated with lasting pain and disability, and considering the prevalence in a young, working population, may lead to decades of impairment. Treatment options vary according to the stage of SLAC, however there is no cure.
Current literature has focused on joint mal-tracking as a potential underlying mechanism leading to SLAC. However, other studies have demonstrated that some malalignment within the joint is tolerated, without arthritic progression. More recently, research is pointing towards the subchondral bone as potential contributors to the pain experience due to the nerves and blood vessels (vascularity) that supply the bone. However, these two biomarkers (joint contact and subchondral bone), have not been the topic of interest in SL research.
How will the team study the problem?
We propose to prospectively and retrospectively analyze quantitative changes in subchondral vBMD in a cohort of patients with unilateral SL injuries. 60 participants will be recruited for our study; n = 30 with a current, unilateral SL injury (prospective cohort) and n = 30 with a previous SL injury (retrospective cohort; 5+ years post injury), through the Hand and Upper Limb Center (HULC) at St. Joseph’s Hospital. All participants will undergo both static and dynamic CT scans of the hand and wrist. Participants will also be asked to fill out patient-reported questionnaires related to pain and disability, as well as quantitative sensory testing to document pain threshold. The images from the CT scan will be used to create joint contact maps and to obtain subchondral bone density values. From there, we will determine the correlation between joint contact, subchondral bone density, and patient-reported outcome measures with the hopes of better understanding pain and disability following an SL injury.
Cited Sources
Shah CM, Stern PJ. Scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) wrist arthritis. Curr Rev Musculoskelet Med. 2013;6(1):9-17. doi:10.1007/s12178-012-9149-4
Murphy BD, Nagarajan M, Novak CB, Roy M, McCabe SJ. The Epidemiology of Scapholunate Advanced Collapse. Hand. 2020;15(1):23-26. doi:10.1177/1558944718788672
O’Meeghan CJ, Stuart W, Mamo V, Stanley JK, Trail IA. The natural history of an untreated isolated scapholunate interosseus ligament injury. J Hand Surg Am. 2003;28(4):307-310. doi:10.1016/S0266-7681(03)00079-2
Lalone EA, MacDermid J, King G, Grewal R. The Effect of Distal Radius Fractures on 3-Dimensional Joint Congruency. J Hand Surg Am. 2021;46(1):66.e1-66.e10. doi:10.1016/j.jhsa.2020.05.027
Rainbow MJ, Wolff AL, Crisco JJ, Wolfe SW. Functional kinematics of the wrist. J Hand Surg Eur Vol. 2016;41(1):7-21. doi:10.1177/1753193415616939
Burnett WD, Kontulainen SA, McLennan CE, Hunter DJ, Wilson DR, Johnston JD. Regional depth-specific subchondral bone density measures in osteoarthritic and normal patellae: In vivo precision and preliminary comparisons. Osteoporos Int. 2014;25(3):1107-1114. doi:10.1007/s00198-013-2568-2
[Closed] Radial Deviation Imaging
The Evaluation of Scaphoid Kinematics Using Four-Dimensional Computed Tomography
We wanted to know how a healthy wrist bone (called the scaphoid) moves when the wrist undergoes radioulnar deviation (waving the hand from the thumb side to the little finger side).

What is the problem?
The scaphoid relies heavily on surrounding tissues for support to coordinate normal wrist bone (carpal) motion behavior [1]. In particular, traumatic injury of the scapholunate ligament (SLL) is known to lead to long-term degenerative arthritis, referred to as scapholunate advanced collapse (SLAC) [2]. Current diagnostic tools for SLL injuries are limited to X-rays and clinical examinations, which are unable to detect subtle bony movement abnormalities; in particular, the latter relies heavily on clinician experience and thus, is subjective [3-5]. X-ray imaging methods are unable to detect dynamic instabilities, which are early markers of scaphoid instabilities, but their detection could lead to earlier diagnosis and surgical intervention [5]. However, four-dimensional computed tomography (4DCT) can capture abnormal bony movements by measuring carpal motion in real time. The purpose of this study was to use 4DCT as a method of measuring scaphoid centroid translation during radio-ulnar deviation in a clinical setting.
How did the team study the problem?
Twelve participants with no history of wrist pain or injury were recruited and underwent imaging of the dominant wrist using a 4DCT scanner while performing three cycles of radioulnar deviation (8 seconds each) beginning in radial deviation (thumb side). Models of the scaphoid (a wrist bone) and radius (a bone in your forearm) were made at three points in motion: maximum radial and ulnar deviation; and neutral, the position in which the long axis of the middle finger and that of the radius were parallel. The motion was described as the position of the centroid of the scaphoid relative to the position of the radius, such that the motion of the scaphoid was isolated even if the participant moved their arm slightly in the scanner.
What did the team find?
The average scaphoid translation was 1.7 ± 1.5 mm towards the back of the hand, 5.5 ± 1.4 mm towards the fingers, and 2.3 ± 0.9 mm towards the thumb (6.4 ± 1.3 mm total) such that the scaphoid extended from extreme radial deviation to extreme ulnar deviation. There was no statistically significant difference in scaphoid translation between lunate type nor sex.
How can this research be used?
This data provides a starting point for establishing normal scaphoid motion in healthy subjects, which can be compared to individuals with wrist injuries and used to advance the understanding of the complex motion of the carpals. These findings augment a clinicians’ ability to provide better patient diagnoses and treatment. This study can also validate 4DCT as a diagnostic tool for wrist injuries whose symptoms are minimal and dynamic, and therefore missed by current static diagnostic techniques. Lastly, a better understanding of wrist motion can lend itself to innovations in wrist implant design, creating an implant which can mimic native wrist movement.
Cautions
Further research needs to be done to obtain significant, distinguishing results about the entire wrist as only one bone and one outcome measurement was analyzed in this study. I would like to acknowledge that I am not a medical professional. Any findings presented here are suggestions based on the findings of this research.
References: This research was conducted as part of Sydney Robinson’s (M.E.Sc, Western University) Master’s research in Biomedical Engineering. The complete study protocol and results will be published on the Western University Electronic Thesis and Dissertation Repository upon completion of her degree.
Cited Sources:
[1] C. Padmore, H. Stoesser, G. D. Langohr, J. Johnson, and N. Suh, “Carpal Kinematics following Sequential Scapholunate Ligament Sectioning,” J. Wrist Surg., vol. 08, no. 02, pp. 124–131, 2019.
[2] R. Lane and M. Varacallo, “Scapholunate Advanced Collapse ( SLAC Wrist ),” StatPearls Publishing LLC., 2019. .
[3] S. W. Wolfe and J. J. Crisco, “Mechanical evaluation of the scaphoid shift test,” J. Hand Surg. Am., vol. 19, no. 5, pp. 762–768, 1994.
[4] S. W. Wolfe, A. Gupta, and J. J. Crisco, “Kinematics of the scaphoid shift test,” J. Hand Surg. Am., vol. 22, no. 5, pp. 801–806, 1997.
[5] I. S. Mat Jais and S. C. Tay, “Kinematic analysis of the scaphoid using gated four-dimensional CT.,” Clin. Radiol., vol. 72, no. 9, pp. 794.e1-794.e9, Sep. 2017.
[Closed] Hand Forces and Golf Grip Study
The Evaluation of Different Golf Grip Designs and Their Impacts on Individuals Hand Forces with and without Hand Arthritis
We wanted to know if ‘arthritic’ designed golf grips allow individuals with hand arthritis to better grip a golf club by reducing the hand forces when swinging the club.

What is the problem?
Arthritis is the most prevalent, incurable disease in Canada affecting 1 in 5 individuals over the age of 15 [1]. It commonly affects the hands causing pain, swelling, stiffness, and approximately a 15% limitation in one’s grip flexion and extension capabilities [2]. Golf is a low-impact, dynamic sport that assists both younger and older individuals in maintaining a healthy and active lifestyle. As the hands are the only contact point between the player and the club, the design of the golf grip greatly influences a golfer’s grip. Several ‘arthritic’ designed golf grips have been developed and marketed for older golfers who have difficulties gripping and swinging a golf club. However, these grips lack the quantitative evidence to support their claims of providing support and assistance to golfers with hand arthritis.
How did the team study the problem?
A newly developed Grip Configuration Model used to measure grip flexion percentage, was paired with the Finger Tactile Pressure Sensors (FingerTPS), wireless finger force measurement system designed by Pressure Profile Systems (PPS, Los Angeles, CA, USA). A sample of 27 golfers of all skill levels (17 healthy golfers and 10 with hand arthritis) were evaluated for their grip flexion percentage and finger force of their bottom gripping hand. Twelve golf grips were evaluated with nine being standard golf grip designs manufactured by Golf Pride, and three arthritis grips designed by Lamkin, Tacki-Mac, and Winn.
What did the team find?
It was found that the participants with hand arthritis had a 45% limitation in their maximum golf grip strength capabilities compared to the participants who did not have hand arthritis. In 11 out of the 12 golf grips tested, the individuals with hand arthritis exhibited higher grip forces when swinging than their maximum golf grip strength capabilities, whereas the healthy participants exhibited roughly a 30% lower overall grip force. This is an alarming observation as exerting large grip forces could cause further harm to already damaged joints. The grips which generated the lowest grip forces for the participants with hand arthritis and the healthy participants was the soft firmness (CP2 Pro) jumbo sized grip, and the soft firmness (CP2 Pro) mid-sized grip, respectively. Therefore, the commonality between the individuals with and without hand arthritis was that the soft firmness, larger diameter designed grips generated the lower hand forces and required the least amount of grip flexion in both test groups. For the ‘arthritic’ designed golf grips, the Lamkin arthritis grip generated the second lowest grip force in the individuals with hand arthritis. However, for the healthy group this grip generated the third highest grip forces. Overall, these findings suggest that standard and ‘arthritic’ designed golf grips may cause excessive grip forces in golfers with hand arthritis. Therefore, there is no clear indication that ‘arthritic’ designed golf grips are beneficial to golfers with hand arthritis.
How can this research be used?
The results of this research can be used to assist researchers, clinicians, golfers, and golf grip manufacturers to better understand the mechanics of hand arthritis in relation to golf and other racquet or bat-and-ball sports. With this understanding, golf manufacturers will be better equipped to design and develop evidence based ‘arthritic’ golf grips for golfers with hand arthritis which will reduce the hand forces and percentage of grip flexion required.
Cautions
Further research needs to be conducted in this area to obtain significant, distinguishing results. I would like to acknowledge that I am not a golf teaching instructor or medical professional. Any findings that have been present here are suggestions based on the findings of this research.
References: This research was conducted as part of Sara Holland’s (M.E.Sc, Western University) Master’s research in Mechanical and Materials Engineering. The complete study protocol and results of Sara Holland’s Master’s thesis titled: Investigating Grip Range of Motion and Force Exerted by Individuals with and without Hand Arthritis during Functional Tasks and while Swinging a Golf Club [2] has been published on the Western University Electronic Thesis and Dissertation Repository and can be accessed here: https://ir.lib.uwo.ca/etd/6214/
Cited Sources:
[1] Arthritis Society, “The Trust About Arthritis,” 2018. [Online]. Available: https://www.arthritis.ca/about-arthritis/what-is-arthritis/the-truth-about-arthritis. [Accessed: 22-Dec-2018].[2] S. F. Holland, “Investigating Grip Range of Motion and Force Exerted by Individuals with and without Hand Arthritis during Functional Tasks and while Swinging a Golf Club,” Western University, 2019.
[Closed]Evaluation of Individual Finger Forces during Activities of Daily Living in Individuals With and Without Hand Arthritis
We wanted to know which activity of daily living required the largest exertion of force by each finger segment comparing people with and without hand arthritis.

What is the problem?
In Canada, 1 in 5 individuals over the age of 15 are affected by arthritis [1]. Osteoarthritis is the most prevalent, incurable form of the disease commonly affects the hands causing pain, swelling, stiffness, and limitations in one’s grip strength and range of motion [1]. A variety of joint protection programs and assistive devices have been developed to provide support and independence to individuals with hand arthritis. However, joint protection handbooks such as Kleinert et al. [2] are not evidence based and consist of activities that are no longer relevant in today’s modern society such as using a pencil to dial a rotary phone. Therefore, the purpose of this study was to use a commercially available sensor system (FingerTPS, Pressure Profile Systems, Los Angeles, CA, USA) to determine the envelope of applied forces during some common activities of daily living in healthy individuals and those with hand osteoarthritis.
How did the team study the problem?
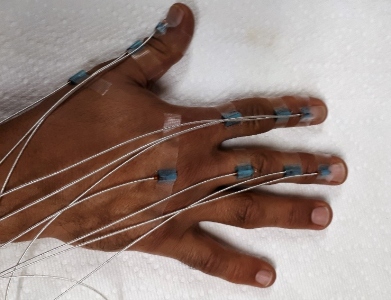
To measure the forces at the fingertips, a commercially available finger force measurement system was purchased. The Finger Tactile Pressure Sensor System (FingerTPS) is a wireless, capacitive measurement system designed by Pressure Profile Systems (PPS, Los Angeles, CA, USA). Encompassed into comfortable, flexible finger cots, they were easily able to slip over the participant’s dominant hand thumb, index, middle, and ring finger. A sample of 46 participants (25 healthy: 21 with hand osteoarthritis) were recruited for this study. A variety of 17 tasks involving the hands were selected from various aspects of daily life including kitchen tasks, cleaning tasks, dressing and grooming tasks to include a combination of common power and precision grips. Each task was performed two consecutive times in an uninstructed, natural manner that the participants would normally complete the task.
What did the team find?
It was found that for the precision gripping tasks of buttoning a shirt and plugging in a toaster for the healthy participants demonstrated the largest peak forces in the thumb ranging from 9.6 ± 1.0 N to 34.8 ± 1.6 N, respectively. For the participants with hand osteoarthritis, the maximum force ranged from 7.9 ± 1.8 N by the thumb during the shirt button task and 30.7 ± 3.7 N by the thumb during the plug in task. However, the difference between the participants with and without hand osteoarthritis was seen in the precision task which demonstrated the smallest average peak forces. For the healthy participants this was in the turning of a key task with a range of 1.4 ± 0.6 N in the ring finger, where the participants with hand osteoarthritis demonstrated a 2.9 ± 0.7 N force range by the ring finger during the writing sentence task. Tasks which utilized a power grip, the largest and smallest average peak force was demonstrated by the scissor task. The ring finger demonstrated the largest force (4.4 ±1.8 N) where the index finger demonstrated the smallest force (3.2 ± 0.7 N). This was also true for the participants with hand osteoarthritis with the largest peak force demonstrated by the index finger (4.8 ± 1.4 N) and the smallest peak force demonstrated by the thumb (2.3 ± 1.0 N).
How can this research be used?
This research can be used to further progress the area of hand arthritis research in order to gain a better understanding of the mechanics of the hands when performing activities of daily living. Further measurements of forces applied by the fingertips would add to the accuracy of current biomechanical models of the hand and measuring the forces in other finger segments would shed valuable insight as well. This knowledge could then be used by clinicians and manufacturers to develop evidence based joint protection programs and device to help individuals with hand arthritis regain their independence and reduce the progression of their arthritis. Future work should also examine forces applied by the hand during other applications such as recreation, sport, and vocational (work) tasks.
Cautions
In using the FingerTPS sensors, for this current study protocol only the forces at the fingertips were measured losing valuable information about the applied forces to various finger segments, namely the middle and proximal phalanges of each finger. There was also a large disparity in age between the two cohorts, with a generally young sample of healthy individuals and a much older sample of participants with hand osteoarthritis. This is likely a compounding factor in the difference in force reported as grip strength tends to decrease with age.
References: This research was conducted as part of Mike Riddle’s (M.E.Sc, Western University) Master’s research in Biomedical Engineering.
Cited Sources:
[1] Arthritis Society, “The Trust About Arthritis,” 2018. [Online]. Available: https://www.arthritis.ca/about-arthritis/what-is-arthritis/the-truth-about-arthritis. [Accessed: 22-Dec-2018].
[2] Kleinert Institute, “Joint Protection Program Handbook For People with Arthritis.” Kleinert Kutz Hand Care Center, Louisville, Kentucky, pp. 1–22, 1988.
[Closed] Hand Forces During Activities of Daily Living
The Development of a Novel Finger Kinematic Measurement Technique using Electromagnetic Tracking to Evaluate Activities of Daily Living
We wanted to develop a program that was practical but used the highly sophisticated electromagnetic (EM) tracking system to measure the joint angles of the fingers and determine if these measures were comparable to the more commonly used goniometer.
What is the problem?
Finger kinematics is a common measurement in biomechanics as proper hand function is crucial for many tasks that we complete daily. However, measuring the motion of the finger bones and joints can be complicated as the hand is made up of many bones, operates within a small volume, and moves in a wide variety of manors. This is even more challenging when people have an injury or disease such as hand osteoarthritis. Arthritis impacts 1 in 5 adults in Canada making it the most prevalent, incurable form of the disease commonly affecting the hands causing pain, swelling, stiffness, and limitations in one’s grip strength and range of motion [1]. The most commonly used measurement technique for evaluating the small joints of the hand is a manual goniometer. Yet there are several issues with this technique concerning human error and its ability of only being able to measure two-dimensional static positions, making this technique incapable of evaluating the hands movements during dynamic activities of daily living (ADL). Electromagnetic (EM) tracking technology is a more sophisticated system which can evaluate the three-dimensional dynamic movements of the hand. Electromagnetic tracking technology has not been previously set up for in vitro use to evaluate the small movements of the hand. Therefore, a new six degrees of freedom finger coordinate system was developed to measure the motion pathway of the fingers in the hands when flexing and extending the fingers and when performing ADL.
How did the team study the problem?
In order to study this problem, a new six degree of freedom coordinate system was developed in the MatLab software to appropriately interoperate the EM tracking output measures. The new method was used to examine nine everyday tasks performed by both healthy participants and participants with hand osteoarthritis. Both groups performed the tasks normally and with a clinically used joint protection method. Joint protection programs are recommended to patients who have hand arthritis as they can reduce pain in the joints [1]. However, no quantitative data exists as to their effectiveness, and they have not been updated to reflect current technology. A comparison between the recorded ranges of motion during these tasks was done.
What did the team find?
In this study, the newly developed finger kinematic measurement technique was found to be comparable to finger kinematics measured clinically and is consistent with what is already presented by Coupier et al (2016). In terms of the clinical data, this study showed that the participants with hand osteoarthritis had less total range of motion (flexion/extension) in many of their joints. Participants with hand osteoarthritis also had less range of motion during the key, plug, and bottle tasks in some of their joints. These findings are important as they show that individuals with hand osteoarthritis do perform tasks differently, and that they do have a more limited range of motion in their finger joints. It also shows that while some joint protection recommendations do decrease the range of motion, not all of them do, which may mean that these recommendations need to be updated.
How can this research be used?
This study presents a foundation for finger kinematic evaluation for in vivo use and describes a methodology that will be used for larger studies to be conducted to examine finger kinematics in various clinical and functional applications. This research also has bearing on the study of finger motion in people with different diseases of the hand. Having a way to measure finger motion that is applicable to everyday tasks is important and is the foundation for many more potential studies on finger motion and diseases.
Cautions
The sample size was of concern for this study with a disparity in age between the two cohorts, with a generally young sample of healthy individuals and a much older sample of participants with hand osteoarthritis. The sensor system was tethered to the data acquisition system, making this impractical for take-home studies.
References: This research was conducted as part of Ahmed Tanashi’s (M.E.Sc, Western University) Master’s research in Biomedical Engineering.
Cited Sources:
[1] Kleinert Institute, “Joint Protection Program Handbook For People with Arthritis.” Kleinert Kutz Hand Care Center, Louisville, Kentucky, pp. 1–22, 1988.